HOME > What is ANK therapy?
What is ANK therapy?
① Poisonous bacteria as specific medicine for cancer treatment
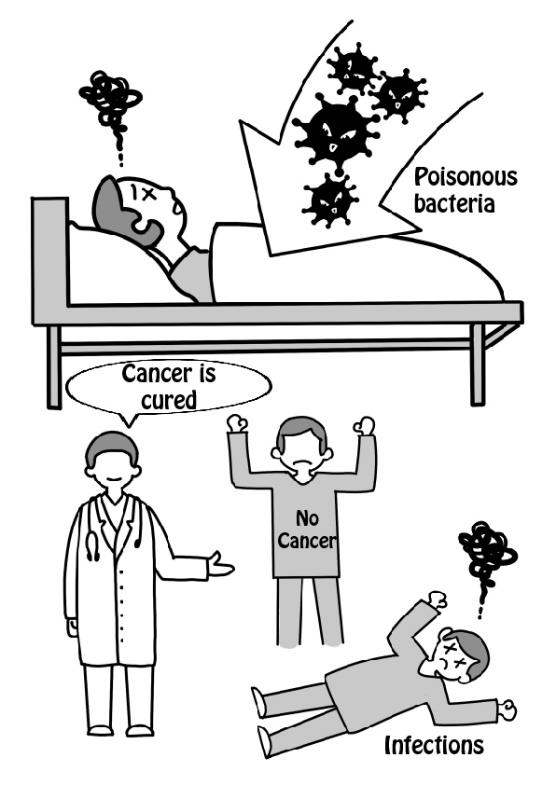
It has been long known concerning the relationship between cancer and immunity that cancers can be cured when contracted with severe acute infections. In the 19th century, a surgeon named Corey performed rough treatments that forced cancer patients to contract strong bacterial infections, and a significant example of its effectivity was seen, and this was published in the scientific journal Nature.
However, a number of patients died from the infections.
The concept of "Corey's poison," symbolized by this experiment, is an important theme in today's immunology.
② The dilemma of effectivity or safety
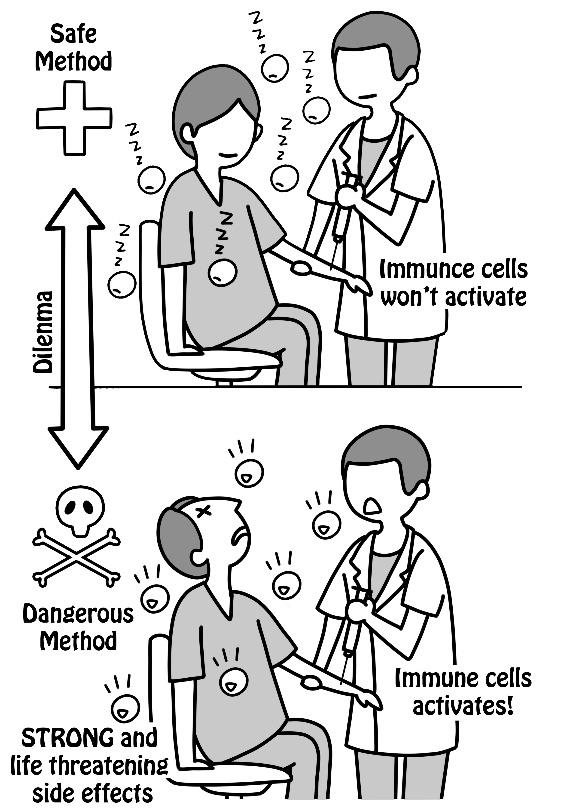
Corey's poison is a dilemma between the following two facts:
■Dangerous stimuli can activate the body's dormant immune system to attack cancer.
■However, if the stimuli is not life-threatening, it is useless (the immune system is not awakened if the stimuli is safe).
To overcome this dilemma, all sorts of stimuli were tried.
③ Immune cells kill cancer cells every day
Based on these studies, the relationship between cancer and immunity has been gradually revealed.
In 1970, Nobel Prize-awarded scientist Lord Barnett said, "Cancer cells occur every day even in healthy people's bodies.
Still, the reason they do not contract cancer as a disease is that the immune cells are constantly monitoring and killing cancer cells as soon as they find them."
Today, this “Immune surveillance System” theory is widely supported.
④ Cancer proliferates when "cancer cells > immune cells"
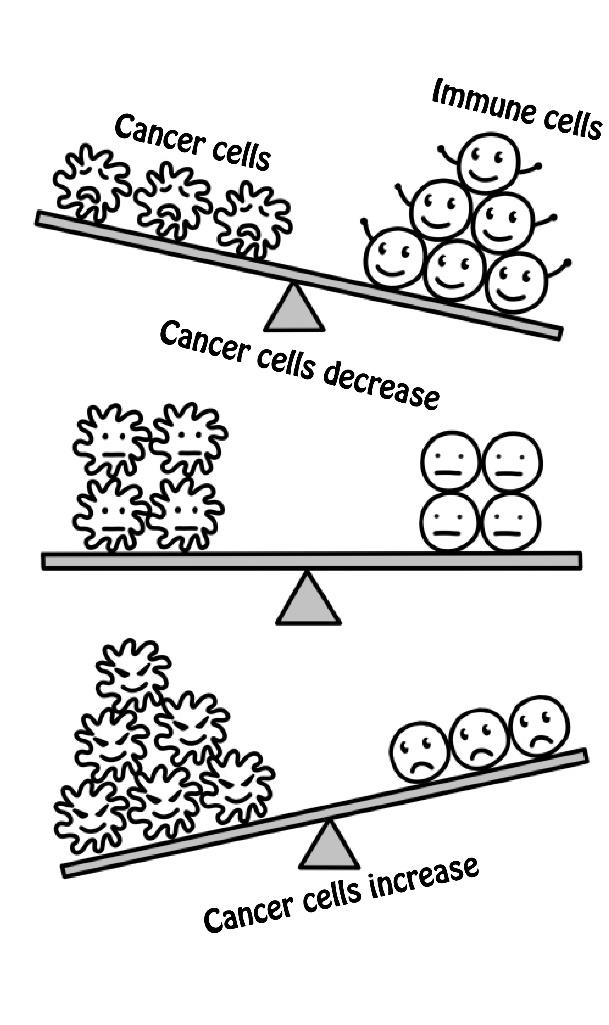
Conversely, when im mune cells that monitor cancer cells aren’t functioning adequately for some reason, the power relationship between the two is reversed, and the cancer cells begin to increase.
Since our immune system has destructive power, such as causing severe inflammation, it is always suppressed by normal cells and immune cells themselves.
If the balance leans further to the suppressive side, cancer cells will not be killed immediately, allowing the growth of cancer.
⑤ Cancer cells pacify immune cells
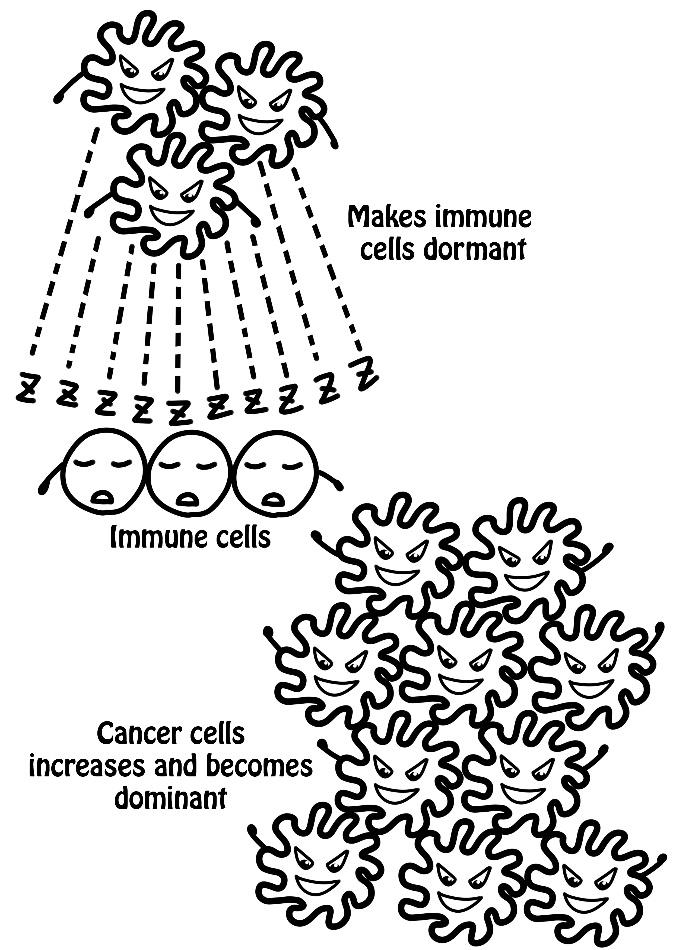
Cancer cells try to make immune cells, which are their natural enemies, dormant. The force is always there, but once the cancer becomes dominant, its power to make the immune cells dormant will get even stronger, and the body will fall into a strong immunosuppressive state. While the immune cells are dormant, the cancer cells keep increasing until the patient is diagnosed with cancer.
Many methods have been tried in order to break through the wall of immunosuppression in cancer patients, but no substance was found to overcome the dilemma of effectivity and safety mentioned above in ②.
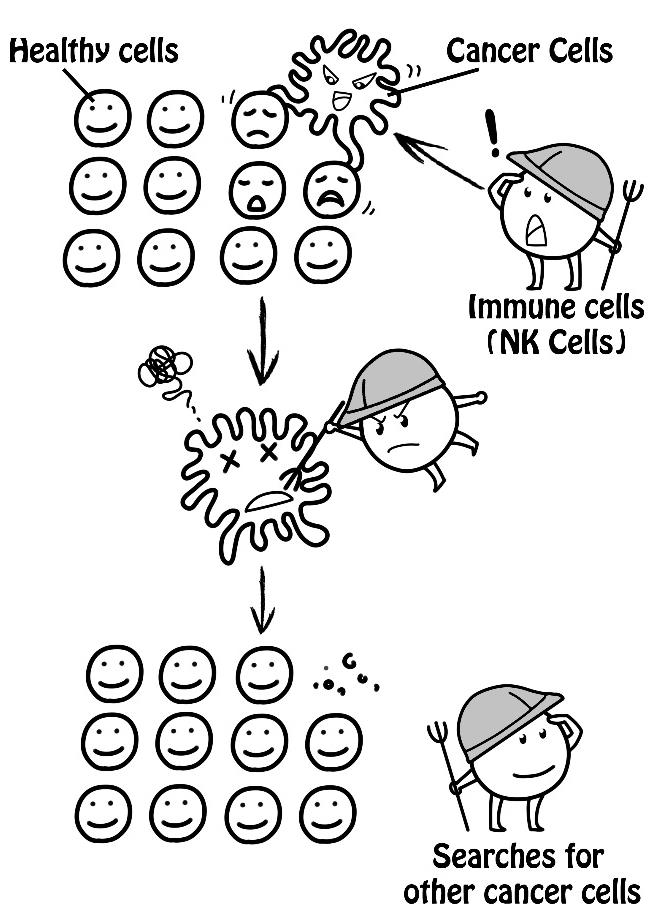
⑥ Discovery of Natural Killer (NK) cells
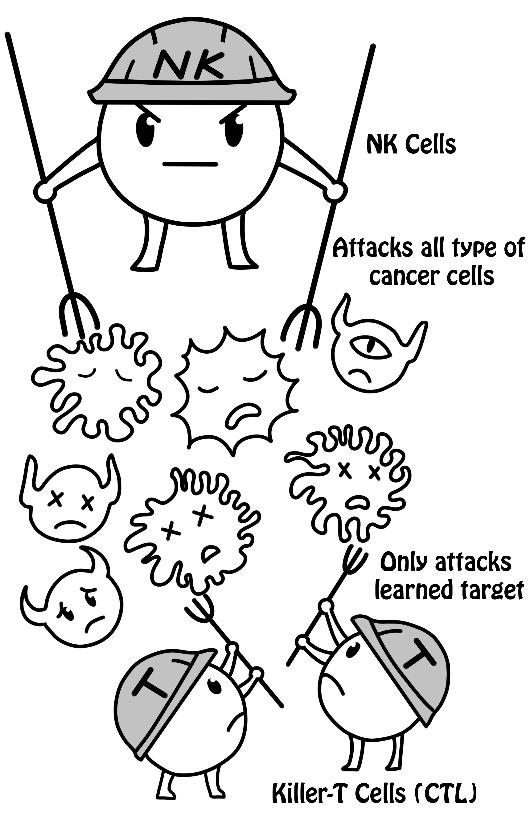
However, in the 1970s, while looking for an aid for the immune monitoring mechanism, researchers discovered that cancer cells died in rapid succession when they mixed cancer cells with healthy people’s blood. Even when they changed the type of cancer cells, they still died immediately. From this blood, immune cells that had not been known until then were found. Killer T cells, which have traditionally been known to kill cancer, require a learning process to recognize the target and will only attack the learned target.
The newly discovered cells have excellent capabilities beyond Killer T cells and kill any kind of cancer cells instantly without any learning process.
Due to typical (natural) immune behavior, this cell, which works like a killer, was named "Natural Killer (NK) Cell."
⑦ Intense stimulation is required to awaken NK cells
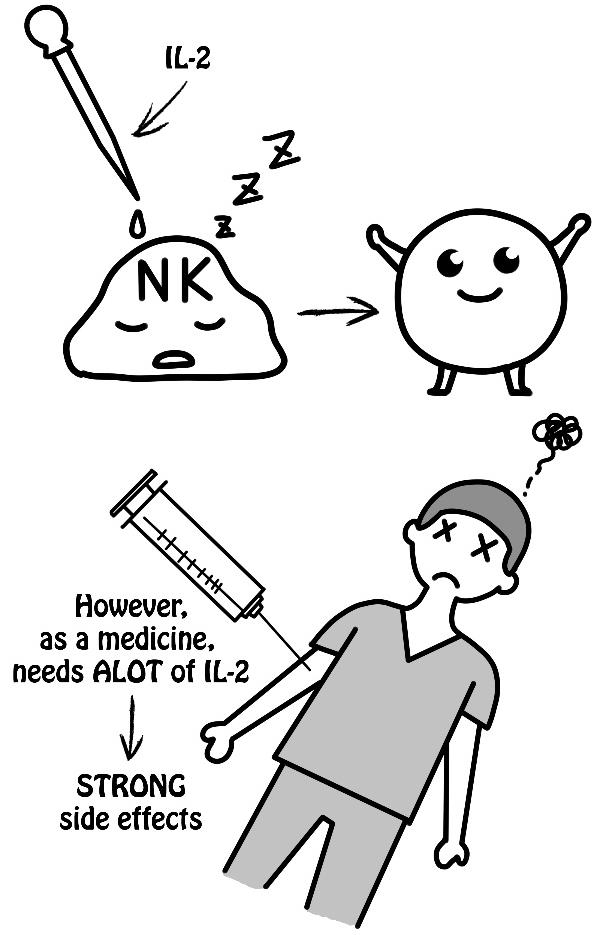
Research on immune cell therapy continued after the discovery of NK cells. Interleukin 2 (IL-2), an immunostimulant secreted in the body, strongly stimulates the NK cells. The mass production of IL-2 became possible with the advent of genetic engineering and was administered to the body as a medicine in repeated experiments, raising expectations as a special remedy for cancer. However, if IL-2 was administered in a safe amount, it was blocked by the wall of immunosuppression and was not effective. It was effective when administered in a large dose, but the patient’s life would be at risk by the strong side effects.
Again, the dilemma of "Corey's poison" remained.
⑧ “Immune Cell Therapy” that stimulates and cultures the immune cells extracorporeally
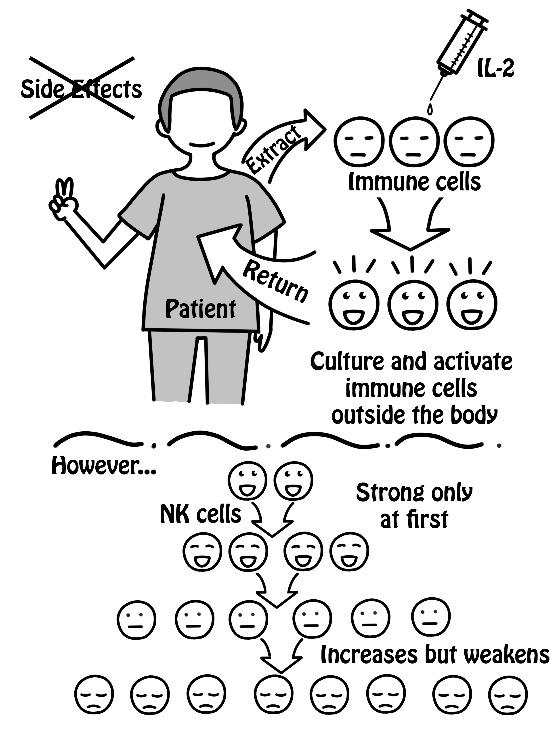
To overcome this dilemma, a treatment that extracts immune cells from the cancer patient, makes the immune cells stronger while cultured outside the body, and returns the cultured immune cells to the patient's body, was devised. Since it is cultured outside the body where immunosuppression does not affect it, immune cells are more likely to grow with fewer restrictions than even inside a healthy person’s body, and can be stimulated without worrying about side effects.
This devised treatment is called “Immune Cell Therapy.”
However, as for NK cells, there is the issue that its activity first increases, but gradually decreases when it continues to proliferate, and a solution to this was needed.
⑨ Large-scale clinical trial conducted in the United States
In 1984, the National Institutes of Health (NIH) conducted a large-scale clinical trial of immune cell therapy.
NK cells’ activity decreases when they continue to proliferate for a long time outside the body. So, in order to ensure a sufficient number of immune cells, a large amount of lymphocytes*, equivalent to the amount included in approximately 50 liters of blood, was extracted, cultured for three days with highly concentrated IL-2, and returned to the body before the number increased too much to the extent that the NK activity decreased (LAK therapy). In this clinical trial, there were significant examples of the effects eliminating large tumors all at once, even if they were progressive cancers that were difficult to treat with standard treatments.
However, due to the tremendous side effects and enormous cost, it was not possible to put into practical use.
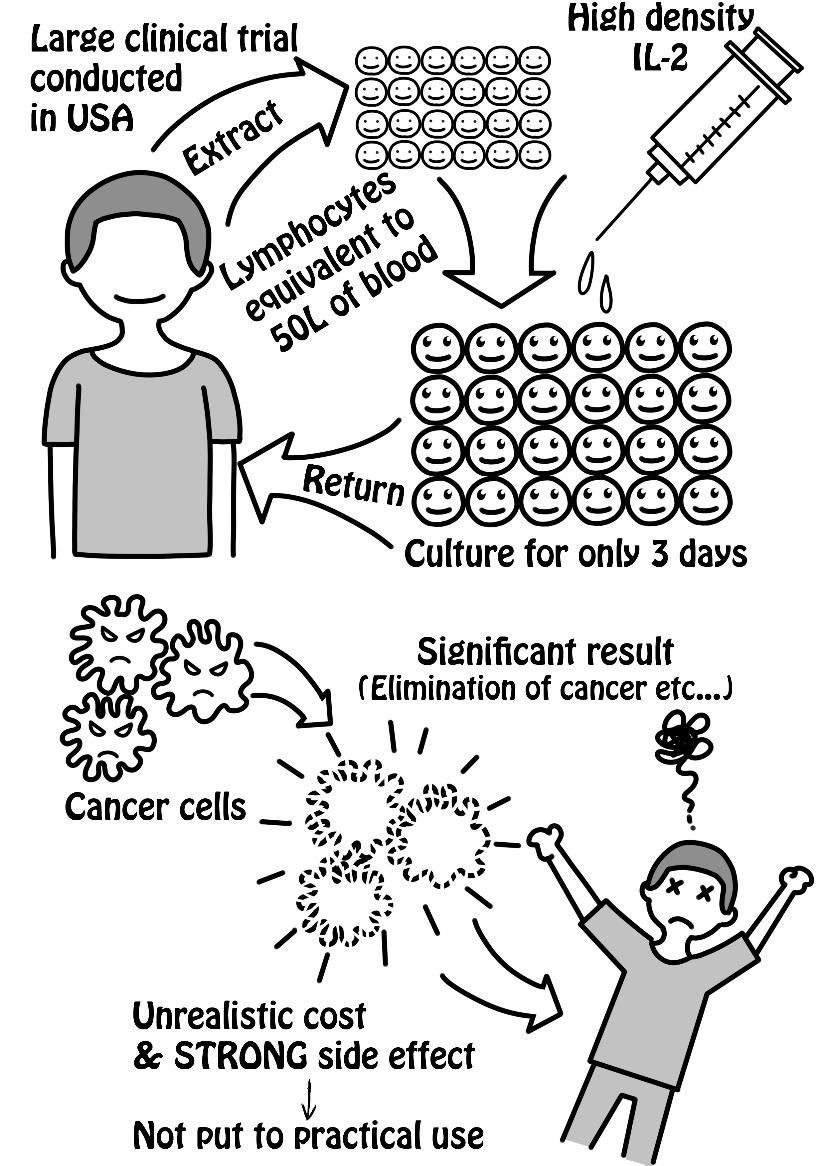
*Precisely, apart from lymphocytes, it also contained other white blood cells. A large number of lymphocytes were collected using a method of separating lymphocytes from continuously extracted blood outside the body, and returning most of the other blood components back to the body sequentially (leukapheresis, hereafter referred to as "lymphocyte separation and collection").
*When a large tumor causes necrosis, a large amount of substances such as potassium dissolves into the body fluid, causing dangers such as CPA (cardiopulmonary arrest).
As a result, the treatment was carried out by occupying the ICU (Intensive Care Unit) and was impractically costly.
⑩ Clearing the challenge, and the birth of Amplified Natural Killer Cell(ANK)Therapy in Japan
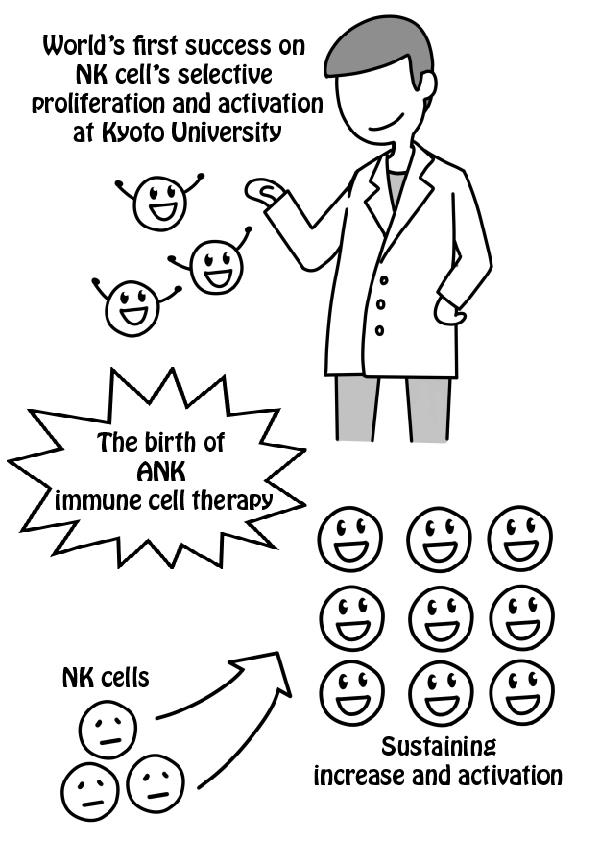
In Japan during the 1990s, experts in immunology at Kyoto University succeeded in full-scale culture of NK cells which researchers around the world had failed at.
By making full use of complex culture technology while carefully determining the condition of NK cells, they succeeded in increasing the number of NK cells (1,000 times or more for healthy subjects) while making NK activity of the cancer patients even stronger than healthy subjects (10 times or more). The treatment that uses this method is called ANK therapy.
⑪ ANK cells’ three roles inside the body
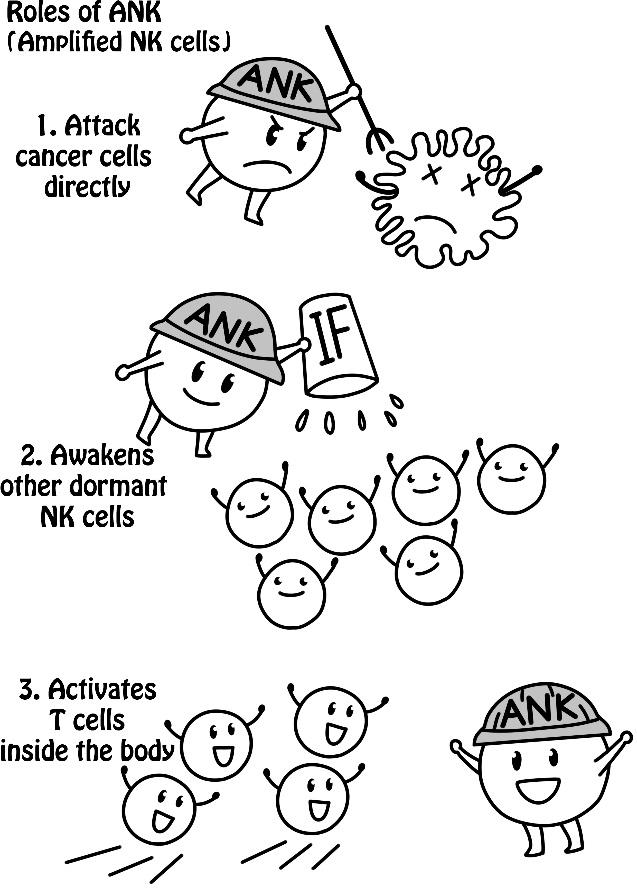
ANK cells that are proliferated and activated outside the body and returned to the patient’s body have the following three effects:
(1) They attack cancer cells directly.
(2) By releasing a large amount of immunostimulant, such as interferon, they awaken the other dormant NK cells inside the body.
(3) They gather Killer T cells and activate them (CTL) as reinforcements.
Approximately 500 million to 1 billion ANK cells are returned to the body at a time, but there are hundreds of times more NK cells in the body. Therefore, high effectivity can be expected when (2) is added to (1).
⑫ Breaking the wall of immunosuppression by repeated treatment
The numerical value indicating the speed at which the NK cells kill cancer cells is called NK activity*. NK activity in cancer patients is very low without exception, but when ANK cells are infused once, NK activity will rise to a level that is even higher than in healthy people.
However, the wall of immunosuppression will push back, causing the NK activity to fall rapidly within a few days. Therefore, by repeating the infusion before the NK activity falls, this treatment will maintain the NK activity at a high level and aim to reach the state in which NK activity does not decrease too much even without infusion. This is the goal of ANK therapy. The infusion counts to reach this goal vary depending on the condition of the patient.
*NK Activity: Estimated by investigating the number of cancer cells killed by letting the collected NK cells and cancer cells fight for a certain period of time under certain conditions.
*The therapeutic strength of ANK Therapy 1 course exceeds the U.S. method mentioned in P11⑨.
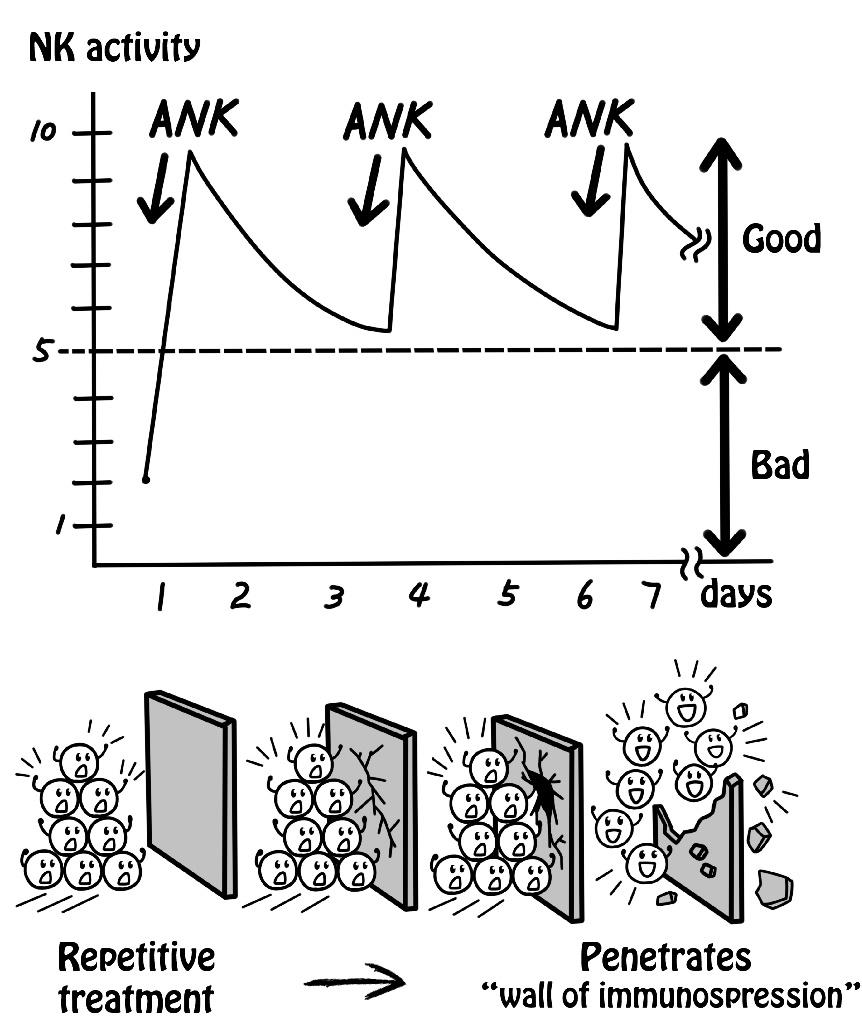
If the proliferated NK cells are returned to the patient’s body at once, a large tumor will cause necrosis and is dangerous. Therefore, ANK performing clinics will divide the treatment into 12 infusions, to gradually penetrate the wall of immunosuppression, in order to make the treatment safe to perform at a clinic.
⑬ Treatment designed to treat progressive cancer on its own
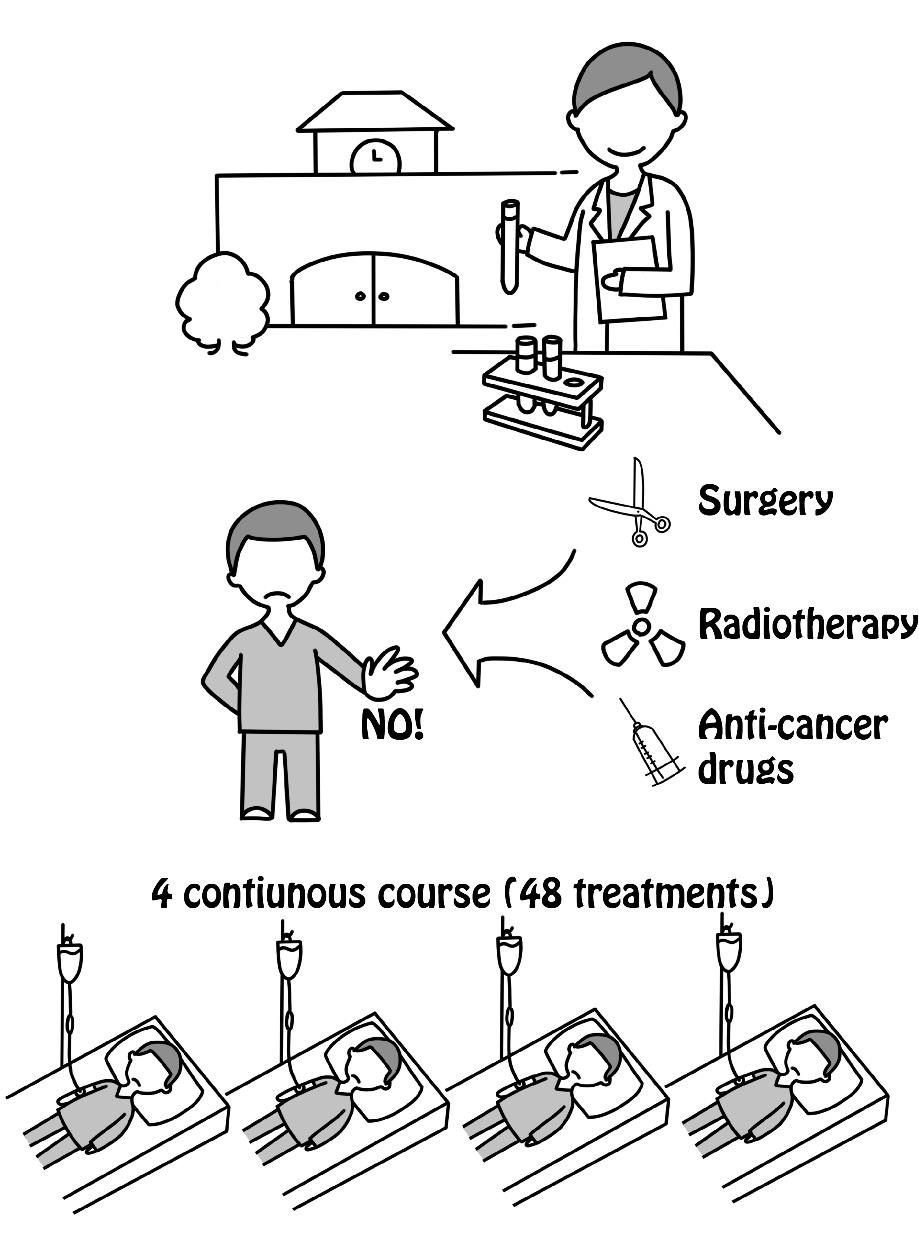
In the 90's, a clinical trial was conducted on ANK therapy, which was at the research stage at that time, at Kyoto University.
Patients with progressive cancer joined this trial under the condition that they would not consider other treatments. In exchange, the ANK therapy was administered continuously without interval for 4 courses (6 weeks) at no cost to the patients.
All the patients, of whom there were more than a dozen, with progressive cancer experienced complete remission and their cancer did not recur for over five years.
After opening the practice to the public in 2001, many terminal phased patients with little or almost no life expectancy, and so called cancer refugees with no remaining standard treatment as a recourse, received this therapy.
In reality, since ANK therapy cannot be performed under conditions ideal for university research, we are currently adapting ANK therapy to various realities, such as appropriate combination with standard treatment.
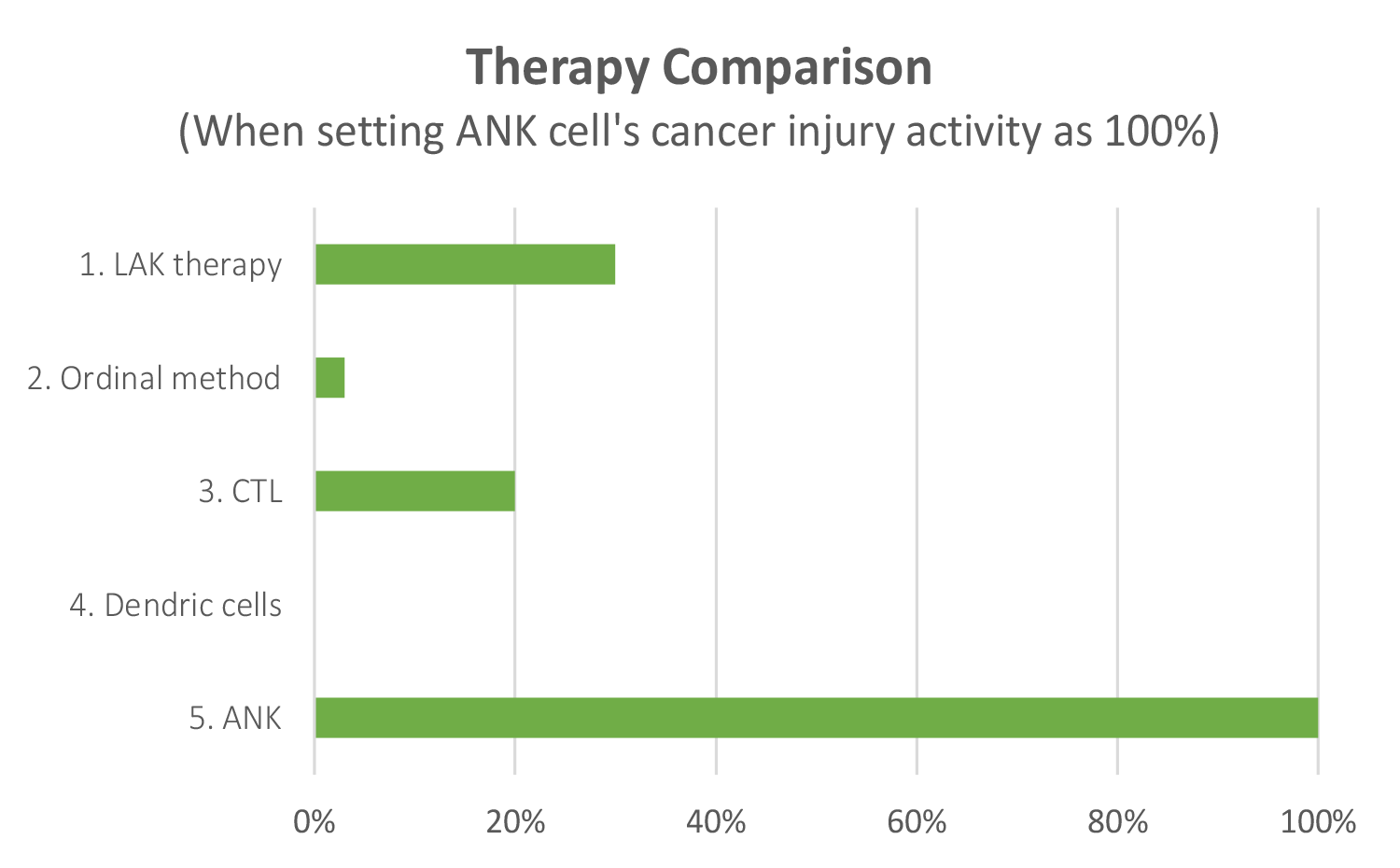
⑭ ANK therapy is completely different from ordinal immune cell therapy
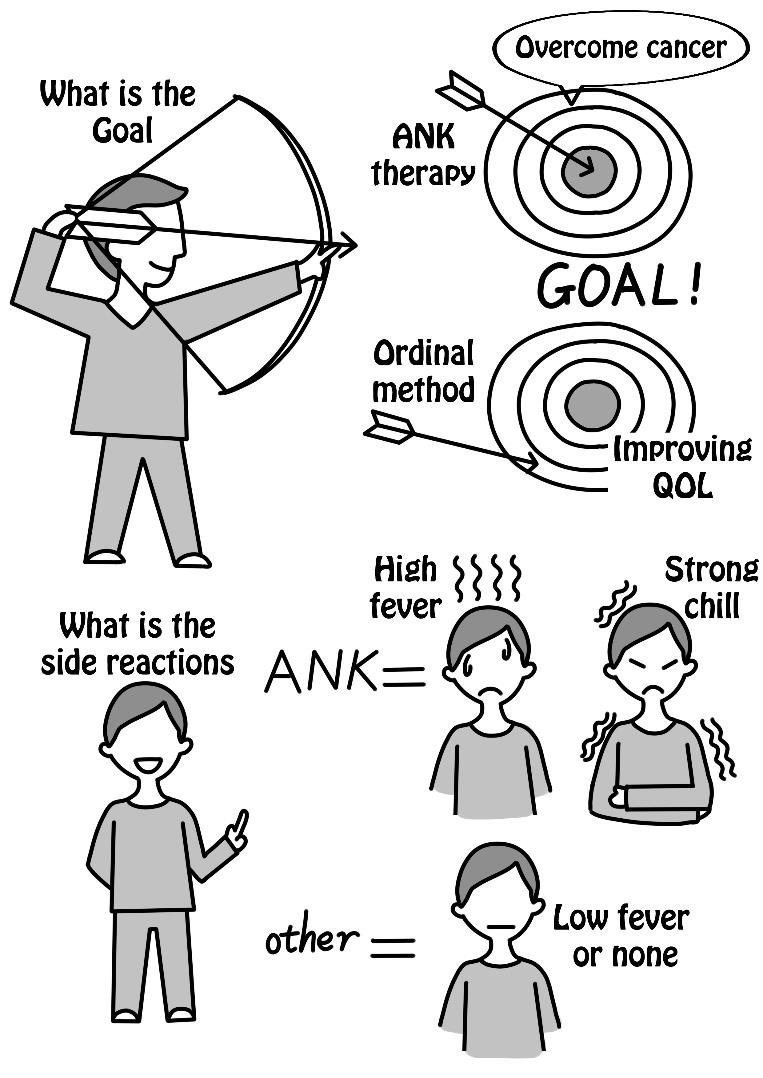
ANK therapy is completely different from the ordinal immune cell therapy* which is currently being performed in Japan. The ultimate goal of the ordinal method is to reduce side effects of people receiving standard treatment, improve quality of life, and extend life expectancy to some extent. The goal of ANK therapy is to overcome progressive cancer. Strong immune side reactions (such as fever) as described in Chapter 2 P27 do not occur with the ordinal method.
These differences are due to differences in the NK cell activity and the number of cells.
*The ordinal method is an extremely scaled down version of LAK therapy which has been confirmed to be effective in the United States. Immune cell therapy in Japan uses ordinal methods or dendritic cells, and has various names with different brands.